In the intricate landscape of healthcare, the concept of informed consent stands as a pivotal guardian of patient rights. This article delves into the profound role that informed consent plays in medical malpractice cases, unraveling its significance, legal implications, and the delicate balance it strikes between patient autonomy and healthcare provider responsibilities.
Unveiling the Essence of Informed Consent
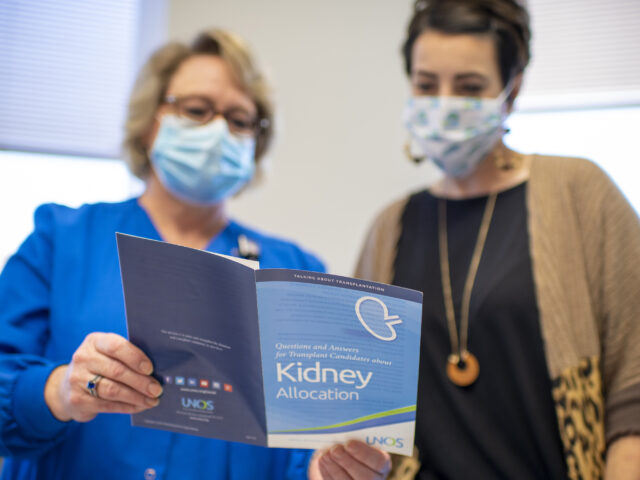
Informed consent, at its core, is more than a mere formality; it is the cornerstone of a respectful and ethical patient-provider relationship. It involves the communication of relevant information to patients, ensuring they comprehend the nature, purpose, risks, and alternatives of a proposed medical intervention. This transparent dialogue empowers patients to make informed decisions about their healthcare, fostering a sense of autonomy and active participation in their treatment plans.
The Legal Tapestry: Informed Consent and Medical Malpractice
In the legal realm, the absence or mishandling of informed consent can give rise to medical malpractice claims. Healthcare providers have a duty to disclose information that a reasonable person would deem necessary to make an informed decision. Failure to fulfill this duty may result in legal consequences, as patients may argue that they were not adequately informed, leading to unforeseen complications.
Medical malpractice cases often hinge on the establishment of negligence. When it comes to informed consent, negligence can manifest in various forms, such as inadequate information disclosure, failure to answer patient queries, or even proceeding with a procedure without obtaining valid consent. Courts scrutinize whether healthcare professionals adhered to the standard of care expected in similar circumstances, emphasizing the importance of transparent communication.
Balancing Act: Autonomy vs. Provider Responsibilities
In navigating the delicate dance between patient autonomy and healthcare provider responsibilities, informed consent emerges as the linchpin. While patients have the right to make decisions about their healthcare, healthcare providers shoulder the responsibility of ensuring that these decisions are based on comprehensive and accurate information.
Clear and effective communication becomes paramount in striking this balance. Providers must tailor their approach to individual patients, considering factors such as their health literacy, cultural background, and emotional state. A personalized approach not only respects patient autonomy but also fortifies the foundations of a trustworthy patient-provider relationship.
Evolving Standards and Challenges
As medical practices and technologies evolve, so do the standards for informed consent. The landscape is witnessing an increased focus on shared decision-making, encouraging collaborative discussions between patients and providers. However, this evolution brings forth its own set of challenges, including the need for healthcare professionals to stay abreast of the latest information and effectively communicate complex medical details to diverse patient populations.
Moreover, the advent of telemedicine adds an extra layer of complexity to the informed consent process. Ensuring that patients grasp the nuances of a virtual consultation requires innovative solutions and a reevaluation of traditional communication methods.
Conclusion: Nurturing Trust and Transparency
In conclusion, the role of informed consent in medical malpractice cases is multi-faceted, encompassing ethical, legal, and interpersonal dimensions. As healthcare continues to advance, the emphasis on transparent communication and shared decision-making becomes increasingly vital. Feel free to visit their page to find out more about understanding malpractice law.
For patients, understanding their rights and actively participating in decisions about their healthcare is empowering. For healthcare providers, adhering to the principles of informed consent not only safeguards against legal ramifications but also nurtures a culture of trust and transparency.


